Device Management
Hardware
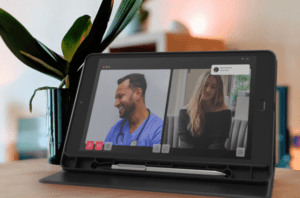
Health
The Emergence of Integrated Technology in Clinical Trials
Decentralized clinical trials (DCTs) represent an increasingly common approach to clinical research that has been accentuated by the logistical challenges presented by the COVID-19 pandemic. The advantages of using digital technologies in virtual clinical trials have become apparent through the development of a wide range of endpoints and specialized mobile hardware features, improvements to the patient experience, tools used for the recruitment and retention of patients, and innovations in trial design.
The key technologies include those concerned with data processing and analysis, including artificial intelligence (AI) and machine learning (ML), wearables, cloud-based management systems that integrate data sources, and mobile technology used for data capture, processing, and storage. Mobile solutions developed by providers like Mason have been crucial in facilitating the rapid expansion of DCTs.
The Rise of Decentralized Clinical Trials
The development of digital technology in recent decades has opened opportunities for the decentralized clinical trial model. In 2011, Pfizer conducted what it claimed to be the first virtual clinical trial, in which an investigational new drug (IND) application gathered all data from participants using electronic devices. But while the growth of drug-based interventional DCTs was minimal in the following years — 7 percent CAGR from 2014 to 2019 — this figure increased to 77 percent from 2019 to 2020 as a result of the pandemic restrictions and increased demand for virtualization.
Currently, integrated technologies for clinical trials from a range of eClinical solutions are brought together in a single platform that draws on electronic data capture (EDC) from clinical research and interactive response technologies (IRT). Integrated voice response (IVR) is an example of an IRT. These different sources and services can be managed through clinical research management systems (CRMS) and electronic patient-reported outcomes (ePROs) that address the high demand for information sharing and access in the clinical research context.
Deregulation
The FDA altered regulations concerning the practices of clinical trials in 2020 in response to the greater demand for virtualization caused by COVID-19 restrictions. FDA Chief Stephen Hanh recognized this as “an acceleration of where we were headed before”. But even so, regulations remain a barrier to the development of innovation in clinical trials where regulatory frameworks such as the General Data Protection Regulation (GDPR) are concerned.
A recent study showed that while digital technologies in clinical trials have the potential to streamline and improve processes, there is still the need for regulatory oversight and continuous development.
The Benefits of Using Integrated Technology with Clinical Trials
Integrated technologies develop and improve clinical research and clinical trial operations in various respects.
- Researchers can access various sources of data in real-time. The integration of different data sources and types of clinical data means access is immediate and can include EDC, IRT, and centralized laboratory data. Immediate access results in the ability to reduce errors and data redundancy.
- The expenses of clinical trial operations can be significantly reduced. There is a greater focus for biopharma companies on keeping costs to a minimum without negatively impacting quality. Travel time and costs are also saved by both patients and sponsors/contract research organizations (CROs).
- Improved efficiency, flexibility, and scalability. Integrated solutions that can combine various technologies, such as IVR and IRT, enable clinical research to adapt to the changes when necessary. The end-user is no longer required to log in to multiple systems but can have full access to trial management and randomization in a single solution.
- Assured reliability and quality of data. Integrated solutions can enable centralized data to meet specified standards and are audit-ready. Redundant data that leads to inefficiencies can be eliminated and IRT data immediately transferred to the EDC system.
How Technological Advancements Support Clinical Trial Processes
Technological advancements as they relate to supporting clinical trial processes are developing many different ways at once. Let’s take a look at some of the most promising advancements developing today.
Artificial intelligence (AI) and Machine Learning (ML)
These technologies can be used to address the gaps and inconsistencies in real-world evidence (RWE) that may be collected through clinical trials or electronic health records (EHRs). However, it is important to avoid bias in the source data as this may be transferred to the AI and ML models. The Ministry of Health in Singapore applies machine learning techniques to data collected from thousands of COVID-19 patients. This makes it possible to detect patients with the virus before symptoms can be detected and without the need for testing.
Wearable Devices
There are many forms of wearable devices that have been used to capture data for use in clinical trials, including smartwatches, bracelets, patches, fabrics, and wearable sensors. These can be used for tracking physical activity, heart rate, oxygen saturation, sleep, haptics, and perspiration, among other things. Smart bracelets were used to measure step counts in a study of patients going through surgery for advanced abdominal cancer, which found that lower step counts led to a higher risk of unplanned hospital readmission during inpatient recovery.
Electronic Clinical Outcome Assessment (eCOA)
eCOA includes a range of tools that are used to capture data for clinical trials, including the use of various internet-enabled devices for sharing data, such as smartphones and tablets, as well as wearables and sensors. The different forms of eCOA include patient-reported outcomes (ePRO), clinician-reported outcomes (eClinRO), and observer-reported outcomes (eObsRO). Performance outcomes (ePerfO) refer to particular tasks for patients to perform. Mason is a provider of mobile infrastructure solutions for various use cases, including healthcare, and has a range of tools that facilitate eCOA and ePRO use cases.
Online tools
Fox Trial Finder is an online tool developed by the Michael J. Fox Foundation for Parkinson’s disease, which sources volunteers for clinical trials relating to conditions that include Parkinson’s disease and Multiple System Atrophy. There are challenges in falsely reported data and patients who have not been clinically diagnosed, but experts suggest that large samples of data make it possible to identify potential inaccuracies. It is also possible to verify patient information by connecting with electronic medical records.
Continued Enhancements within Clinical Trials
The Clinical Trials Transformations Initiative (CTTI) provides some recommendations for sponsors or CROs, including that feasibility studies are conducted before digital technologies are implemented in clinical trials. As digital devices, infrastructure, and data analytics and management continue to develop, the shift towards the paradigm of decentralized, patient-centric clinical trials is set to continue. Challenges remain in data security, privacy, and regulation, but the groundbreaking capabilities that integrated technology brings to clinical research can be easily noticed.
Mason provides a range of software and hardware solutions that improve clinical trial capabilities. Get in contact with us today to learn how we can advance your project in clinical research.